Critical Bioengineering
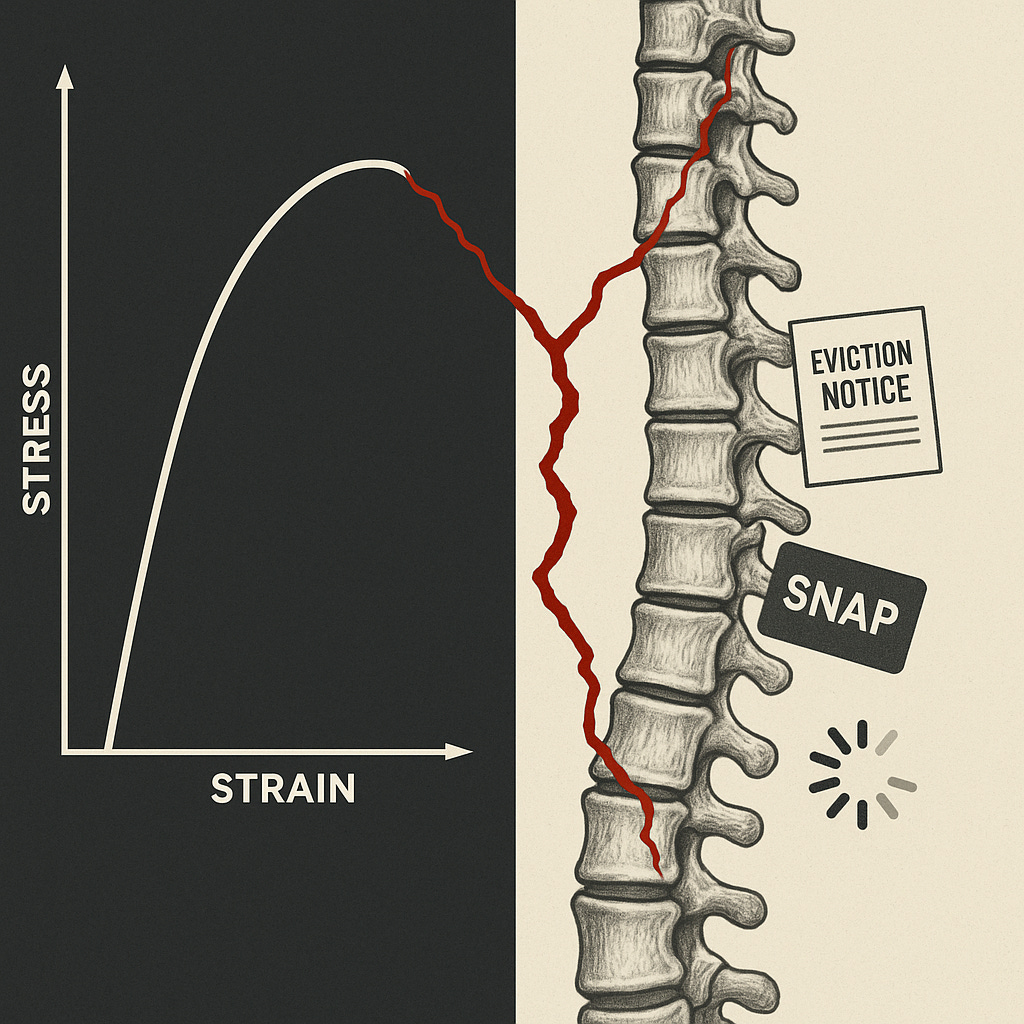
From medical implants to insurance portals, from stress fractures to eviction notices—the physics of failure hasn’t changed. What’s changed is the scale of the harm.
I was trained to see the world in terms of load, stress, and failure.
At Georgia Tech, studying biomedical engineering, I learned that when you design anything that touches the human body, you ask one unforgiving question: When stress arrives, who carries it?
A prosthetic hip must distribute force across the femur. A cardiac stent must scaffold an artery against collapse. A ventilator must assume the work of damaged lungs. Each device gets tested against the same principle: does it bear the load, or does the body?
But when I left the lab and entered the real world—first at Epic Systems implementing hospital records, then at Doximity building tools for millions of physicians, later as CEO of Andwise helping doctors navigate financial stress—I kept seeing the same physics at work in places I didn’t expect.
The decisive “engineering” of health wasn’t happening with scalpels or implants. It was happening in portals, scheduling software, insurance claims, and contracts.
And when those systems failed, the load didn’t vanish into a dashboard. It landed—hard—in bodies.
The Body Keeps Score (And It’s Not Metaphorical)
Seriously: the body is the most reliable instrument we have for measuring the quality of our systems.
Eviction or threat of eviction is associated with elevated blood pressure and cardiovascular stress1
SNAP benefits running out at month’s end? Emergency departments see predictable waves of hypoglycemia admissions2
Algorithmic scheduling that optimizes labor costs over sleep consistency? Workers develop measurable metabolic dysfunction3
At Andwise, I saw this pattern in brutal clarity. Financial stress didn’t just live on balance sheets—it manifested as insomnia, hypertension, burnout. The graphs looked disturbingly like the stress-strain curves from engineering school.
The body, in effect, is a dashboard readout of our bioincompatible institutional design.
In engineering, we map failure modes—the predictable ways a device can break. Working in healthcare systems, I kept meeting their institutional twins:
Single-Point Failures: One crack dooms an implant. One missed form cascades into catastrophe. Benefits systems where a single data entry error can terminate life-sustaining resources.
Brittle Interfaces: A ceramic hip shatters under unexpected stress. So does a benefits portal with rigid deadlines, or employment contracts that punish any deviation from algorithmic perfection.
Seamless Opacity: A device can look perfect while hiding fatal flaws. Same with automation that erases every seam for appeal, correction, or human override—creating a smooth pipeline from process to harm.
These aren’t random glitches. They’re predictable failure modes of systems optimized for throughput, not survivability.
Critical Bioengineering: A Grammar for Redesign
If institutions fail like engineered devices, then they should be held to the standards of competent engineering. This is what I call Critical Bioengineering.
The specifications are straightforward:
Build absorbers, not nets. Safety nets catch you after you fall. Shock absorbers prevent the fall. Design systems that anticipate stress and absorb it—like continuing healthcare coverage automatically during appeals, or unemployment benefits that don’t require weekly re-certification during crises.
Design for fault tolerance. No single missed input should end a life. Build in redundancy, grace periods, and ways to “fail gracefully” rather than catastrophically.
Prioritize the interface. Every interaction between a person and an institution is a load transfer point. Complexity isn’t neutral—it’s a tax on people who can least afford it.
Preserve productive roughness. “Seamless” often means no recourse. Institutions need visible seams—places where humans can pause, appeal, refuse, and correct. These aren’t bugs; they’re essential safety features.
We ought to build things people can survive, yeah?
What’s Coming
We’re entering an era of load multipliers: climate shocks, AI automation, financial fragility, institutional legitimacy crises. All of these are increasing the stress on already-brittle systems.
Traditional engineering solved this problem decades ago. Critical systems in aerospace, nuclear power, medical devices—they’re designed with multiple redundancies, fail-safes, and fault tolerance. They assume stress will arrive and engineer to absorb it.
It’s time we held our social infrastructure to the same standard.
What institutional failures have you felt in your body? What would fault-tolerant social systems actually look like?
Related Reading:
Hoke et al. (2021) in “The Health Impacts of Eviction: Evidence from the National” aggregate evidence linking housing instability (including eviction processes) to elevated blood pressure, weight gain, and worsened cardiovascular indicators. They note that housing instability (including eviction) is associated with elevated blood pressure in observational studies.
Vásquez-Vera et al. (2017) systematic review The Threat of Home Eviction and Its Effects on Health finds that multiple studies report that people living under the threat of eviction report poorer self-rated physical health, including hypertension / high blood pressure.
Aborode et al. (2022) Threats of evictions in the USA: A public health concern outline that even before actual loss, eviction threats are associated with increased incidence of high blood pressure and other physical illnesses.
There is good evidence of monthly cyclical hypoglycemia admissions tied to SNAP exhaustion in low-income populations. Seligman et al. (2014), “Exhaustion of Food Budgets at Month’s End and Hospital Admissions for Hypoglycemia”, is the canonical study. They analyze inpatient admissions in California over 2000–08 and find that among low-income populations, admissions for hypoglycemia are 27% higher in the last week of the month compared with the first week.
Basu et al. (2017) “The Monthly Cycle of Hypoglycemia” further explores temporal patterns of hypoglycemia and finds that periods of increased SNAP benefit disbursement are associated with reduced end-of-month hypoglycemia risk in lower-income populations.
Ye et al. (2023), “Association between Shift Work and Metabolic Syndrome”, study a cohort of 1,211 male manufacturing workers over 4 years. They find shift work (versus day work) associated with increased risk of metabolic syndrome — and longer shift work history (>20 years) amplifies this risk.
Cheng et al. (2021), “Night shift work and the risk of metabolic syndrome”, using data from Taiwanese hospital workers, find that night shift work is associated with elevated risk of metabolic syndrome (adjusted OR ~1.36) and specifically with high waist circumference and high blood pressure components.