Temporal Injustice in Medical Residency Programs
Medical residency is mythologized as a rigorous yet fair process that molds future physicians into competent, compassionate practitioners. Protected by duty-hour regulations, accreditation standards, and oversight mechanisms, it is framed as a system grounded in professionalism, equity, and skill development. Yet this narrative conceals a starkly different reality. Residency thrives on unrecognized labor, entrenched inequities, and a culture that enforces silence to maintain the status quo.
Far from an equitable system, residency is engineered to extract labor under the guise of education, systematically reinforcing privilege and perpetuating hierarchies. The costs of this exploitation extend beyond the individual trainee, compromising patient care and undermining the very principles residency claims to uphold.
Examining residency through the framework of temporal justice—which views time as a finite, shared resource manipulated by systems of power—illuminates how its design is not flawed but intentionally exploitative. Reforming this system requires more than superficial fixes; it demands a complete restructuring centered on care, equity, and accountability.
Residency’s dysfunctions are best captured in shadow logs—informal records maintained by residents to document their lived experiences. These logs reveal how residency systematically exploits its workforce while upholding inequitable and exclusionary practices.
1. Unpaid Labor: The Backbone of the System
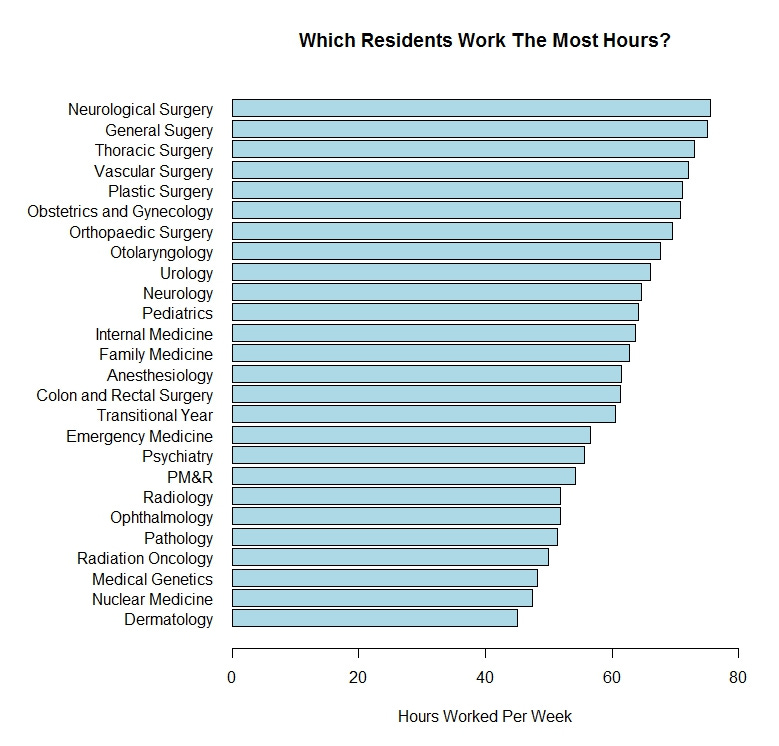
Residency is sustained by the erasure of unpaid and invisible labor. Duty-hour regulations cap weekly hours at 80, but these limits are routinely violated. Residents frequently complete critical tasks—charting, patient follow-ups, care coordination—off the clock. This hidden labor props up hospital systems while remaining unacknowledged in official records, allowing institutions to avoid hiring sufficient staff.
The Evidence
84% of residents admit to falsifying their hours to meet reporting requirements (Journal of Graduate Medical Education).
Residents contribute an estimated $6 billion annually in unpaid labor, equivalent to the salaries of nearly 70,000 additional healthcare workers (AAMC).
Resident Voices
“If I logged all my hours, it would trigger a violation, so I just stopped reporting them.”
“I spend my ‘day off’ catching up on notes because there’s no time during the week.”
Implications
Chronic overwork leads to resident burnout, impairing decision-making and increasing the likelihood of medical errors (The Lancet).
Hospitals avoid investing in sustainable staffing models, effectively treating residents as a disposable workforce.
This exploitation of labor is not a bug in the system—it is a cornerstone of its design, prioritizing cost savings over ethical training practices.
2. Gatekeeping Opportunities: Reinforcing Structural Inequities
Despite promises of equitable training, residency perpetuates significant disparities in access to career-defining experiences. High-value opportunities, such as complex procedures, leadership roles, or prestigious rotations, are allocated unevenly, often reinforcing existing racial, gender, and socioeconomic inequities.
The Evidence
Women in surgical specialties perform 25% fewer complex procedures than their male colleagues (Journal of Surgical Research).
Black and Latino residents report significantly fewer high-complexity cases compared to white residents, even within the same programs (JAMA Network Open).
International medical graduates (IMGs) are disproportionately relegated to less prestigious rotations and excluded from leadership roles (Annals of Surgery).
Resident Voices
“While others were mentored into high-stakes surgeries, I was routinely assigned minor cases.”
“There was no transparency in how leadership roles were distributed—it felt like favoritism.”
Implications
Marginalized residents face delayed career progression, reduced competitiveness for fellowships, and diminished leadership representation.
The inequitable distribution of opportunities perpetuates medicine’s historical exclusivity, undermining diversity efforts.
These patterns are not incidental—they reflect a system designed to privilege certain groups while marginalizing others, ensuring that hierarchies remain intact.
3. Retaliation Against Advocacy: Silencing Change
Residency culture actively discourages residents from speaking out against unsafe practices, inequitable workloads, or systemic inefficiencies. Trainees who advocate for change often face retaliation, including poor evaluations, exclusion from key rotations, or career stagnation.
The Evidence
41% of residents report experiencing retaliation after voicing concerns (Journal of Graduate Medical Education).
Retaliation disproportionately affects women and residents from underrepresented groups, further entrenching inequities (Academic Medicine).
Resident Voices
“When I raised concerns about unsafe staffing levels, my supervisor stopped assigning me to surgeries.”
“I spoke up about inequities in case assignments, and suddenly my evaluations tanked.”
Implications
The culture of retaliation stifles necessary critiques, perpetuating harm to both residents and patients.
Advocacy becomes a privilege reserved for those insulated from systemic consequences, typically individuals in dominant social positions.
This enforced silence protects institutions at the expense of meaningful reform, perpetuating a culture of fear and compliance.
Temporal Justice—A Framework for Systemic Change
Residency’s exploitation is fundamentally tied to the manipulation of time—residents’ hours are treated as an infinite resource to be extracted, rationed, or withheld. Temporal justice offers a lens through which to understand and challenge these dynamics.
Value Residents’ Time: Time spent on training and care must be respected as inherently valuable, free from exploitation.
Ensure Equity in Opportunities: Career-defining experiences must be distributed transparently and equitably, without bias.
Protect Advocacy: Independent oversight bodies must safeguard residents who raise concerns, ensuring accountability for retaliation.
Temporal justice shifts the focus from superficial compliance to systemic accountability, demanding structural reforms that address the root causes of inequity.
Reimagining Residency
Transforming residency requires bold, systemic changes that prioritize education, equity, and care over institutional efficiency.
1. Decouple Training from Labor
Residency programs must prioritize educational goals over hospitals’ staffing needs, ensuring that residents are not exploited as a cost-saving measure.

2. Guarantee Transparent Allocation of Opportunities
Participatory governance structures can ensure that all residents have equal access to high-value cases, leadership roles, and mentorship.
3. Emphasize Competency Over Quotas
Evaluation systems should focus on holistic, patient-centered care rather than procedural tallies, fostering a more equitable approach to skill development.
4. Embed Training in Communities
Community-based training models can align residency with public health priorities, fostering relational care and addressing health inequities.
5. Establish Independent Oversight Bodies
Resident-led organizations should monitor equity, investigate retaliation, and enforce accountability, ensuring that institutions are held to meaningful standards.
Residents deserve a training system that respects their time, acknowledges their contributions, and prepares them to serve patients without sacrificing their own dignity and well-being. The future of medicine, and the integrity of healthcare, depends on it.