How We’re Failing People in Manic States
And what we can do about it, from my personal experiences and research
When someone experiences a manic episode, the current approaches often cause more harm than healing. Responses rooted in control, fear, and misunderstanding—such as dismissiveness, coercion, and shame—leave those experiencing mania feeling abandoned and alone.

In this guide, we’ll break down the most common harmful responses and offer compassionate alternatives that foster understanding and healing, helping people navigate manic episodes with dignity and support.
Harmful Messages People in Manic States Hear—and Their Impact
1. "You’re out of control!" – Instantly Creates Shame
When a person in a manic state is told they're “out of control,” the message they hear is that their emotions are dangerous or unacceptable. This framing compounds feelings of shame, making them feel like their emotional state is a burden to others or that they are inherently problematic.
A better response: “I know this feels intense right now, but you’re safe.” Offering reassurance helps the person feel grounded and lets them know they are not a danger. Safety and trust are key to de-escalating emotions.
Impact: This approach validates their experience while creating a sense of security. As a result, the person may begin to relax, feeling that they don’t need to suppress or hide their emotions, and this can lead to a calmer state.
2. "Calm down, or we’ll call someone" – Escalates Fear
This common threat implies that forceful action will be taken if the person doesn’t comply, whether through hospitalization or involving authorities. Such threats fuel fear and exacerbate the person’s distress, stripping them of autonomy.
A better approach: “What do you need right now to feel supported?” By asking this, you allow the individual to regain control over their situation, promoting collaboration rather than compliance. This question shows that their needs are important and worthy of consideration.
Impact: When people feel empowered to articulate their needs, they experience a sense of control, which can reduce panic and foster cooperation. They are more likely to express what they need, making the situation easier to navigate.
3. "You’re acting crazy!" – Dismisses Their Experience
Stigmatizing language like “crazy” dismisses the complexity of what the person is experiencing. It reduces their emotional state to something chaotic and invalidates their feelings, leading to further alienation.
A better response: “Your feelings are real; let’s work through this together.” This phrase not only validates their emotions but also conveys solidarity. It signals that they are not alone in navigating their experience and that their emotions are not something to fear.
Impact: By feeling seen and heard, the person is more likely to trust you and open up about what they are going through. This can lead to a more honest conversation, reducing defensiveness and fostering a deeper connection.
4. "No one will understand you if you keep acting like this" – Deepens Isolation
This statement reinforces the idea that their emotions are isolating them from others and that they must suppress or hide them to connect with others. This deepens their feelings of loneliness and alienation.
A better approach: “I can see you’re going through a lot right now. Let’s take this one step at a time.” Acknowledging the intensity of their experience without rushing them through it creates a compassionate space for them to process their emotions.
Impact: This approach reduces the pressure to immediately "fix" or suppress their emotions, allowing them to process what they are experiencing at their own pace. It encourages trust and long-term engagement in the recovery process, instead of quick fixes that lead to further isolation.
Why This Matters
Our current responses to mania often push people further into distress. By labeling, threatening, and dismissing those in manic states, we drive them toward shame, self-isolation, and mistrust of both systems and individuals. This approach creates a harmful feedback loop: the more people in mania are treated as “out of control” or dangerous, the more they internalize those narratives, leading to worsened emotional health and often dangerous self-destructive behaviors.
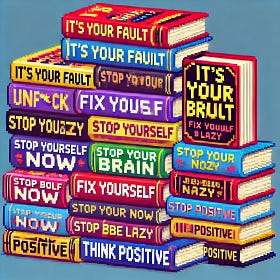
The Hidden Harm in Self-Help
Books like Atomic Habits emphasize the power of small, incremental habit formation. While this approach can help many people build discipline, it often backfires for neurodivergent individuals who struggle with executive dysfunction, motivation, and consistency.
Shifting toward compassionate, non-coercive care can break this cycle. By validating the emotions of people experiencing mania and giving them space to process those feelings, we encourage healing. We help them internalize the understanding that their emotions are real, valid, and manageable, fostering long-term emotional resilience rather than short-term compliance.
A New Way Forward: Compassion and Recovery
To truly help people in manic states, we must fundamentally rethink our approach. Moving from fear-based responses to care models rooted in empathy, autonomy, and support is key. Here’s how we can shift toward meaningful change:
1. Community-Led Support Systems
Peer-led crisis intervention teams, composed of individuals who have lived through manic episodes themselves, can be invaluable. These teams provide immediate, non-coercive support during crises, using de-escalation techniques that prioritize emotional validation over control. Peer-led systems have been shown to reduce the need for hospitalization and police intervention, offering a more humane and compassionate form of crisis care.
Example: In Eugene, Oregon, the CAHOOTS program (Crisis Assistance Helping Out On The Streets) sends mental health workers instead of police for mental health crises, offering an alternative that’s been successful in supporting people without escalation.
2. Proactive Harm Reduction
Providing emotional literacy, mindfulness training, and access to peer support networks equips people with the skills they need to manage their emotions before a crisis occurs. This form of harm reduction focuses on prevention, giving people the tools to recognize their emotional triggers and access support early, before the situation escalates into a full-blown crisis.
Example: Organizations like Hearing Voices Network offer peer support groups where people can share their experiences and learn practical tools for navigating distress without feeling pathologized.
3. Non-Coercive Medical Care
Medical interventions must always be grounded in consent and collaboration. People in manic states should feel like active participants in their care, rather than passive recipients of decisions made for them. Collaborative care means listening to the patient’s experiences and preferences and working together to create a treatment plan that meets their unique needs.
Example: Open Dialogue, a Finnish mental health practice, emphasizes involving the person experiencing a crisis in all decisions about their care, along with their family and close support network. This approach has led to dramatically reduced hospitalization rates.
4. Recovery-Oriented Systems
Mania is often part of a long-term mental health condition. Crisis intervention is just the first step; comprehensive support must continue beyond the immediate episode. This includes providing access to stable housing, job training, and community reintegration programs. Long-term support systems that focus on recovery reduce the likelihood of repeat crises and help individuals build sustainable emotional health.
Example: Programs like Pathways to Housing use a “Housing First” approach to support people with mental health challenges by providing stable housing before addressing other needs, recognizing that security and stability are foundational to recovery.
Why This Should Matter to You
Whether you’ve experienced a manic episode yourself or know someone who has, the pain of being misunderstood or controlled in those moments is profound. This guide is written for those who deserve better—because everyone deserves care that respects their autonomy, validates their emotions, and supports their healing journey.
The good news is that change is possible. By embracing compassionate, non-coercive care, we can build systems of support that empower people instead of punishing them. We can shift from fear-based responses to solutions that foster long-term healing and emotional resilience.
Take Action: How You Can Help
Share this guide with your friends, family, and wider community to raise awareness about compassionate approaches to mania.
Talk to your local officials about implementing peer-led crisis intervention teams in your area.
Advocate for non-coercive mental health care at hospitals, clinics, and community organizations.
Together, we can change how mania is treated and create a future where emotional crises are met with care, not control.